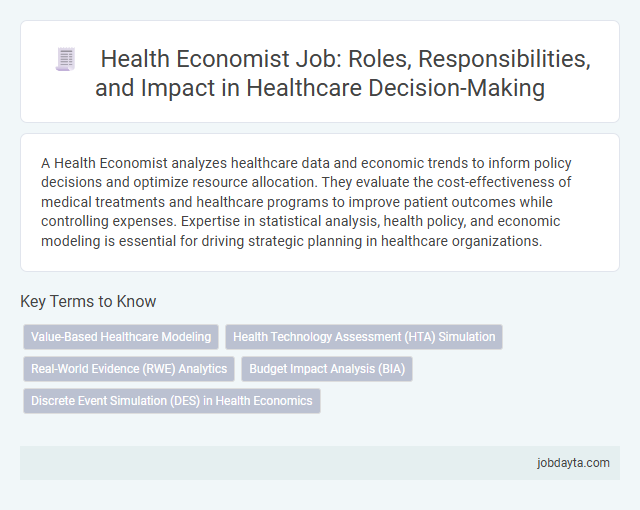
A Health Economist analyzes healthcare data and economic trends to inform policy decisions and optimize resource allocation. They evaluate the cost-effectiveness of medical treatments and healthcare programs to improve patient outcomes while controlling expenses. Expertise in statistical analysis, health policy, and economic modeling is essential for driving strategic planning in healthcare organizations.
Overview of the Health Economist Role in Healthcare
A Health Economist analyzes the financial and economic aspects of healthcare systems to improve efficiency and resource allocation. They evaluate health policies, medical treatments, and public health programs to determine cost-effectiveness and impact on population health. Their work supports decision-making in healthcare organizations, insurers, and government agencies to optimize health outcomes and reduce spending.
Key Responsibilities of Health Economists
Health Economists analyze economic data to evaluate the efficiency and effectiveness of healthcare systems. Their work supports decision-making to optimize resource allocation and improve patient outcomes.
- Cost-Effectiveness Analysis - Evaluate the costs and health outcomes of medical treatments to determine value for money.
- Policy Impact Assessment - Assess economic implications of healthcare policies to guide government and organizational strategies.
- Resource Allocation Optimization - Develop models to prioritize healthcare spending and maximize population health benefits.
Skills and Qualifications Required for Health Economists
| Skills | Qualifications |
|---|---|
| Strong analytical and quantitative abilities | Bachelor's degree in Economics, Health Economics, Public Health, or related fields |
| Proficiency in statistical software such as STATA, R, or SAS | Master's degree or PhD preferred in Health Economics or Health Policy |
| Knowledge of healthcare systems and health policies | Experience with economic modeling and cost-effectiveness analysis |
| Excellent communication and report writing skills | Understanding of epidemiology and biostatistics |
| Ability to interpret complex data and provide policy recommendations | Background in health services research is advantageous |
| Project management and teamwork capabilities | Certification in health economics or related disciplines adds value |
The Role of Health Economists in Healthcare Policy Development
What role do health economists play in healthcare policy development? Health economists analyze data related to healthcare costs, outcomes, and resource allocation to provide evidence-based recommendations. Their expertise helps shape policies that improve efficiency, equity, and access in healthcare systems.
Health Economists and Cost-Effectiveness Analysis
Health economists specialize in evaluating the economic impact of healthcare interventions, ensuring efficient allocation of resources in medical systems. Their expertise supports policy decisions by analyzing costs and health outcomes.
Cost-effectiveness analysis is a core method used by health economists to compare the value of different healthcare treatments. It assesses both the financial costs and health benefits, guiding optimal investment in healthcare services.
Impact of Health Economists on Healthcare Resource Allocation
Health economists analyze cost-effectiveness and efficiency to guide healthcare resource allocation. Their assessments help prioritize funding for treatments and interventions that maximize public health benefits. Understanding their role enables you to appreciate how economic insights improve healthcare decision-making.
Health Economists’ Contribution to Healthcare Innovation
Health economists play a critical role in advancing healthcare innovation by analyzing the cost-effectiveness of new medical technologies and treatments. Their expertise helps healthcare providers and policymakers allocate resources efficiently to improve patient outcomes.
- Cost-Benefit Analysis - Health economists evaluate the economic value of new healthcare interventions to ensure sustainable investment in innovation.
- Policy Development - They contribute to creating evidence-based policies that support innovative healthcare solutions and improve access.
- Resource Allocation - Health economists optimize the distribution of limited healthcare resources by assessing the impact of emerging technologies on system efficiency.
Your understanding of health economists' contributions highlights their essential role in driving actionable insights that foster healthcare advancements.
Challenges Faced by Health Economists in Decision-Making
Health economists play a critical role in guiding healthcare policy and resource allocation through data-driven analysis. Their expertise helps balance cost-effectiveness with quality patient outcomes in complex healthcare systems.
One major challenge faced by health economists is managing uncertainty in clinical data and economic models, which can impact the accuracy of cost-benefit analyses. Another difficulty involves integrating diverse stakeholder perspectives, including patients, providers, and policymakers, to ensure equitable decisions. Limited availability of real-time health data further complicates timely and informed decision-making processes.
Career Pathways and Opportunities for Health Economists
Health economists analyze healthcare systems and policies to improve efficiency and reduce costs. They apply economic theories and data analysis to guide decision-making in healthcare organizations and government agencies.
Career pathways for health economists include roles in research institutions, public health departments, and pharmaceutical companies. Your skills in evaluating health interventions and budgeting can open doors to consulting and policy advisory positions.
Future Trends and the Growing Importance of Health Economists in Healthcare
Health economists play a critical role in shaping the future of healthcare by analyzing cost-effectiveness and resource allocation. The growing complexity of healthcare systems increases the demand for their expertise in policy-making and economic evaluation.
- Data-Driven Decision Making - Health economists use advanced analytics to guide efficient healthcare investments and improve patient outcomes.
- Integration of Technology - Expertise in evaluating digital health innovations and telemedicine enhances economic assessments for emerging healthcare solutions.
- Policy Influence and Resource Management - Health economists support policymakers in optimizing healthcare budgets and ensuring sustainable care delivery models.
Related Important Terms
Value-Based Healthcare Modeling
Health Economists specializing in Value-Based Healthcare Modeling analyze cost-effectiveness and patient outcomes to optimize resource allocation in medical systems. Their work involves developing predictive models that link clinical interventions to economic value, improving both healthcare quality and sustainability.
Health Technology Assessment (HTA) Simulation
Health economists specializing in Health Technology Assessment (HTA) simulation analyze cost-effectiveness and budget impact of new medical technologies using predictive models to inform policy decisions. Advanced simulation techniques integrate real-world data and clinical trial outcomes, optimizing resource allocation and improving healthcare delivery efficiency.
Real-World Evidence (RWE) Analytics
Health economists specializing in Real-World Evidence (RWE) analytics utilize data from electronic health records, insurance claims, and patient registries to evaluate the cost-effectiveness and outcomes of medical interventions in everyday clinical practice. This approach supports healthcare decision-making by providing robust insights into treatment value, resource allocation, and policy development based on real-world patient experiences.
Budget Impact Analysis (BIA)
Health economists specializing in Budget Impact Analysis (BIA) evaluate the financial implications of adopting new healthcare interventions, assessing how these costs affect overall healthcare budgets over short- and long-term horizons. Their analyses incorporate factors such as patient population size, treatment uptake rates, and cost offsets to inform policy decisions and optimize resource allocation within health systems.
Discrete Event Simulation (DES) in Health Economics
Health economists utilize Discrete Event Simulation (DES) to model complex healthcare systems, capturing patient pathways and resource constraints over time to evaluate cost-effectiveness and policy impacts. DES provides granular insights into treatment outcomes, healthcare utilization, and long-term economic implications, supporting evidence-based decision-making in health technology assessments and budget impact analyses.
Health Economist Infographic
 jobdayta.com
jobdayta.com